Facial Bone Fractures
Conveniently located to serve the areas of New York, NY

Dr. Sherman is a recognized expert in facial trauma, and has been teaching the repair and treatment of maxillofacial trauma for over 35 years at The New York Presbyterian Hospital Weill Cornell Medical Center. He is a member of The American Society of Maxillofacial Surgeons and is a co-author of a recognized textbook for the treatment of these injuries. Patients come to him from all over the country and around the world to help reconstruct their facial bones after fractures. Dr. Sherman works with a multi-specialty team to address all the issues and tissues involved within a simple or complex facial fracture: fractures of the maxilla, mid face, sinuses and orbits.
The spectrum of injuries range from the simple (nasal fractures, broken noses) to the repair of complex Le Fort fractures, which will be discussed below. Over the years treatment has evolved from the simple placement of wires to rigid fixation with titanium screws and plates. Imaging has also evolved from simple X-rays to CT scans and 3-D reconstructions which help the surgeon visualize injuries prior to surgery.
Contents
Before and After Photos
Orbital Fractures
An orbital fracture is a traumatic injury to the bones of the eye socket – either the thicker, bony outer rim, the very thin orbital floor beneath the eye, the sides of the orbit, or all. These fractures are generally caused by blunt force, such as a car accident or sports injury, and can impede natural eye movement and functioning.
Symptoms of Orbital Fractures
- Bruising around the eyes
- Double Vision (diplopia)
- Numbness around the eye socket and cheek area extending to upper lip
- Decreased ability to move eye normally (entrapment)
- Sunken appearance of the eye (enophthalmos)
Surgical Examples
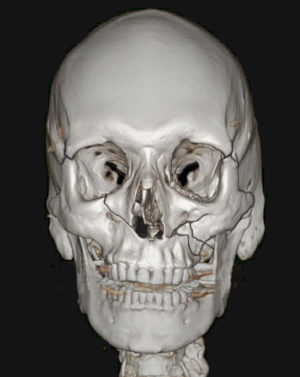
Case 1
Figure A. the patient’s left eye is able to gaze upward, and the right eye is unable to do so due to entrapment of the muscle.
Figure B. shows the orbital floor disparity of both eyes, so that the pupils are at different levels.
Figures C. and D. show the patient postoperatively with the ability to look upward without entrapment, and restoration of the floor so that the pupils are at the same level. Full restoration of ocular movement was obtained, and double vision eliminated.
Case 2
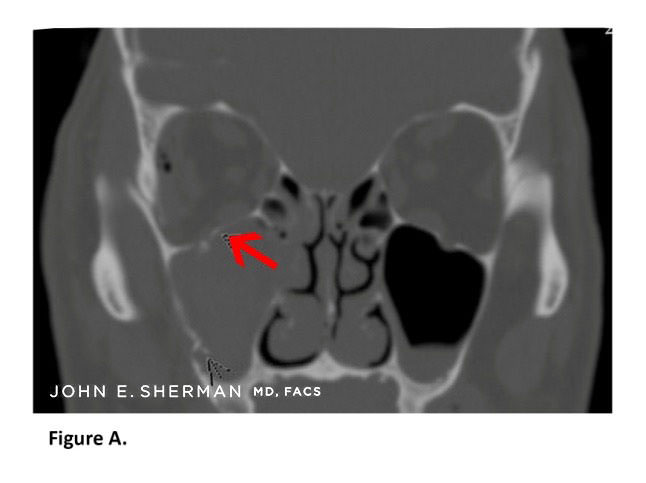
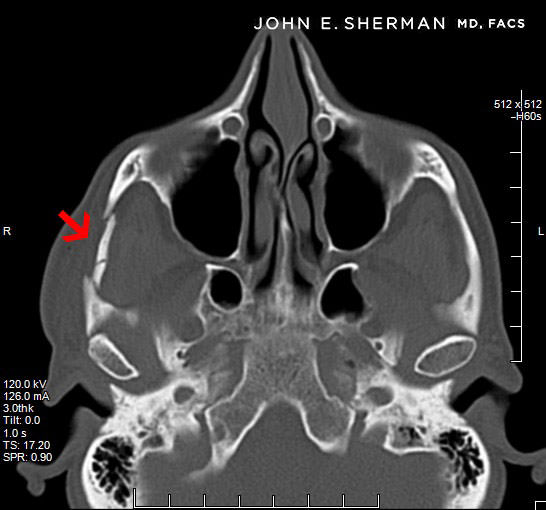
Figure A. Pre-operative scan of 59-year-old patient. Arrow shows displaced orbital floor fracture, occurring in addition to fractures of the maxilla and zygoma.
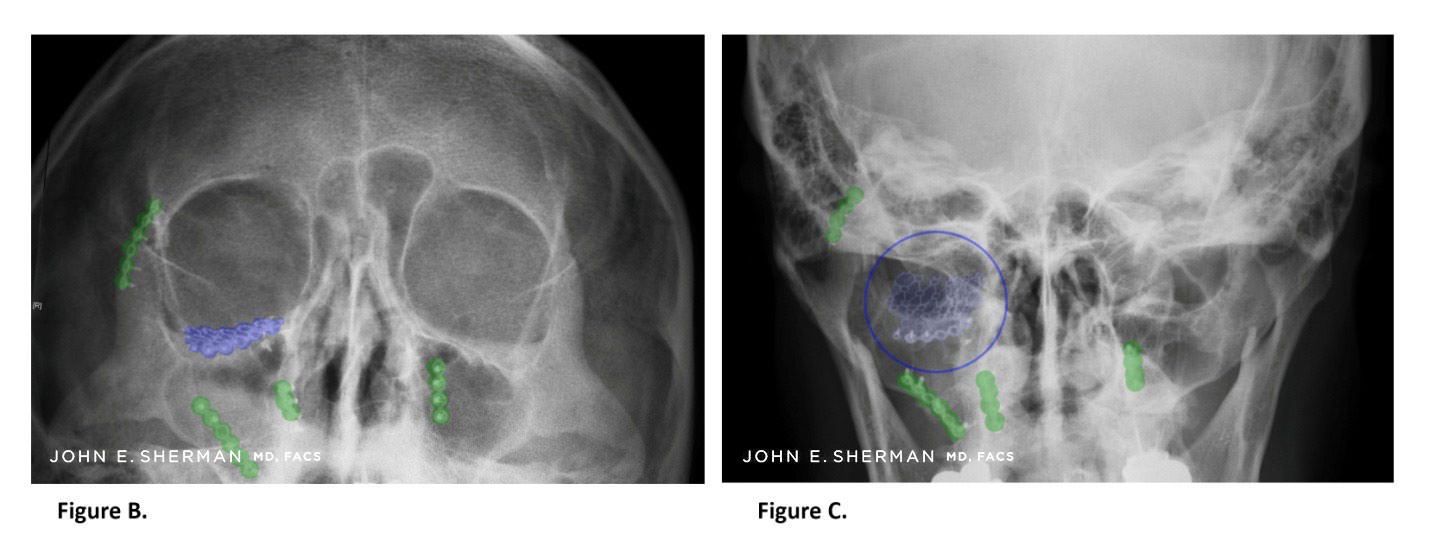
Figure B, C. Restoration of normal anatomy with an orbital floor implant on the patient’s right side – highlighted and circled in blue. Additional plates are on the maxilla and zygoma (cheek bone) – highlighted in green.
Case 3
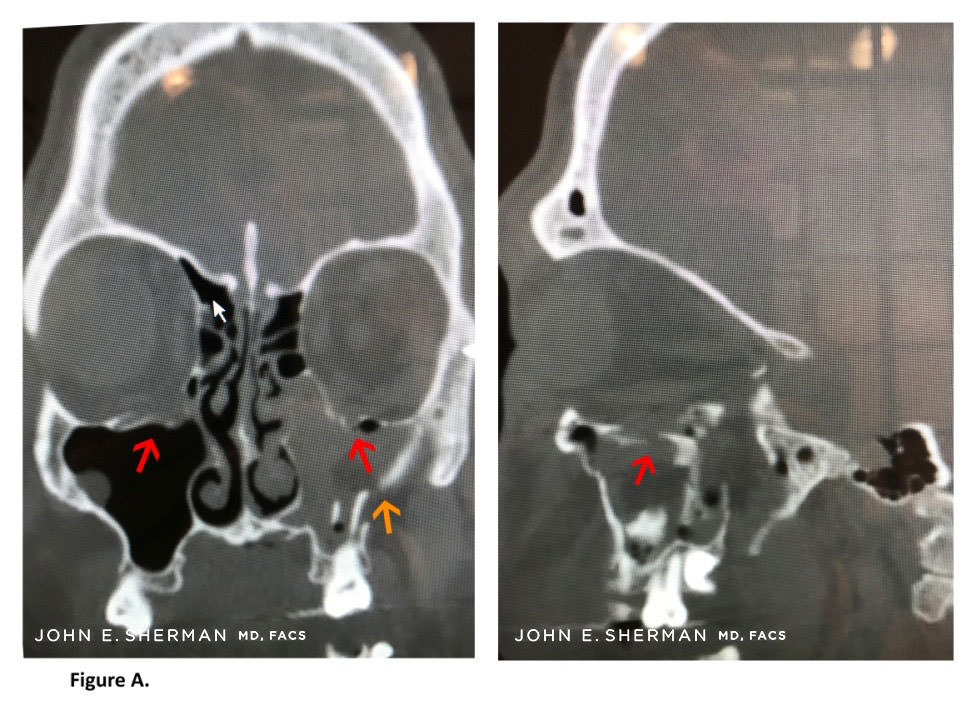
Figure A. Arrows (red) indicate bilateral orbital floor fractures after this 37-year-old patient was assaulted. The patient also has fractures of the left maxilla (orange arrow).
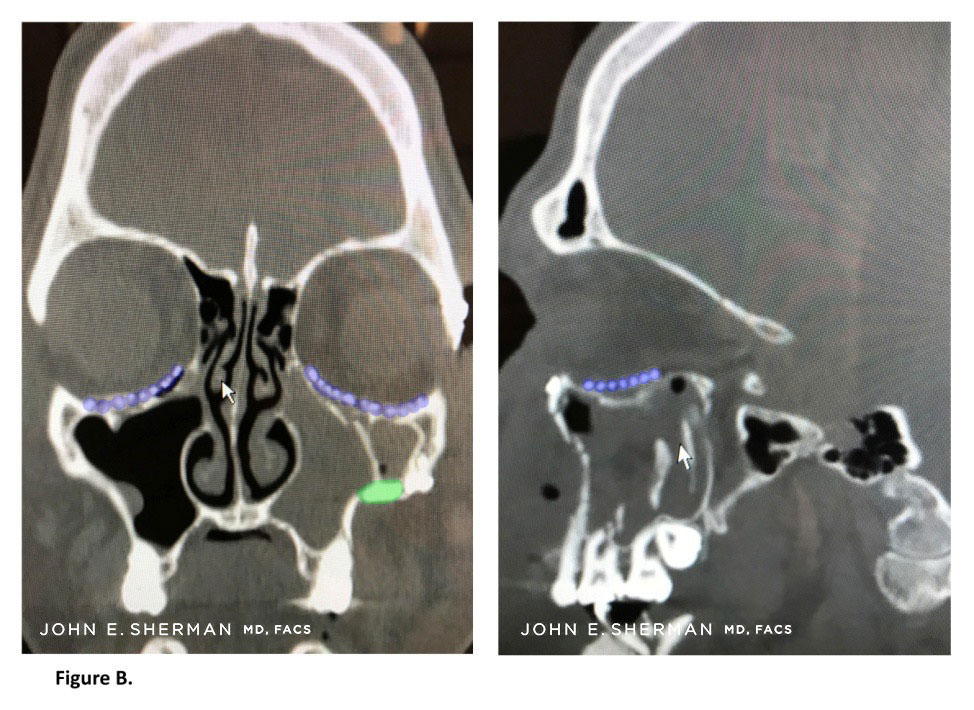
Figure B. Placement of orbital implants (highlighted in blue), correcting the medial wall defects as well as the orbital floors. Additional plate is on the left maxilla (green).
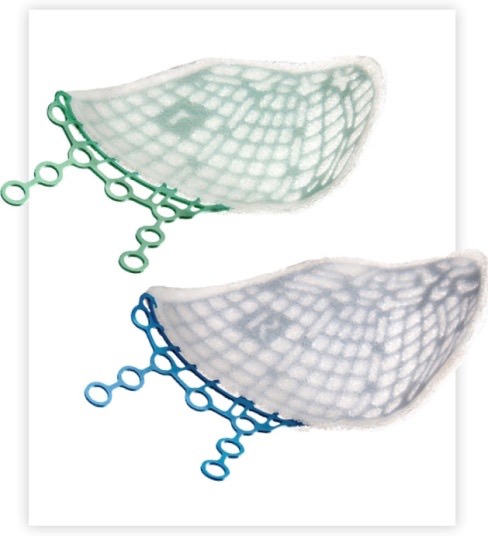
Stryker® Contour Medpor titanium implants that are often used to reconstruct the orbital floor. A small (4mm) screw is secured to the orbital rim for fixation.
Facial Fractures and Cheekbone Surgery (zygoma)
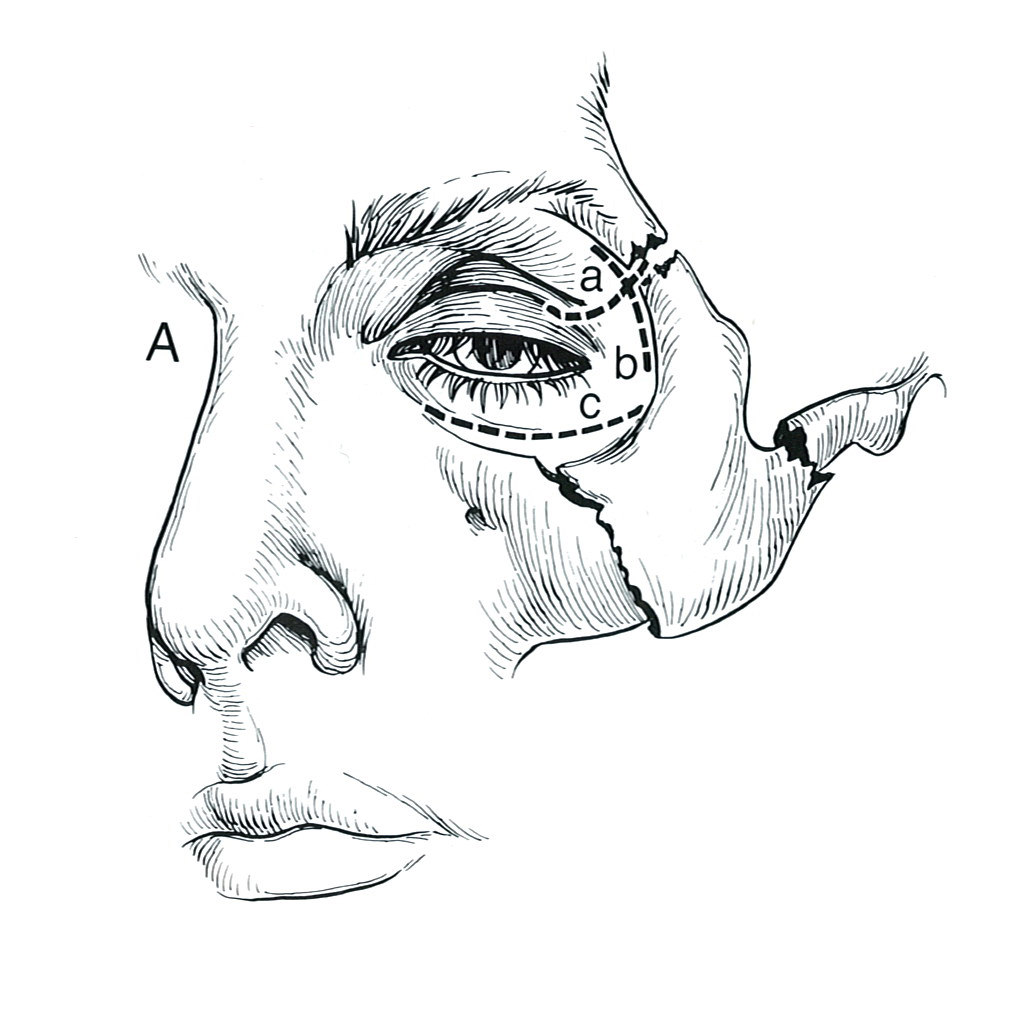
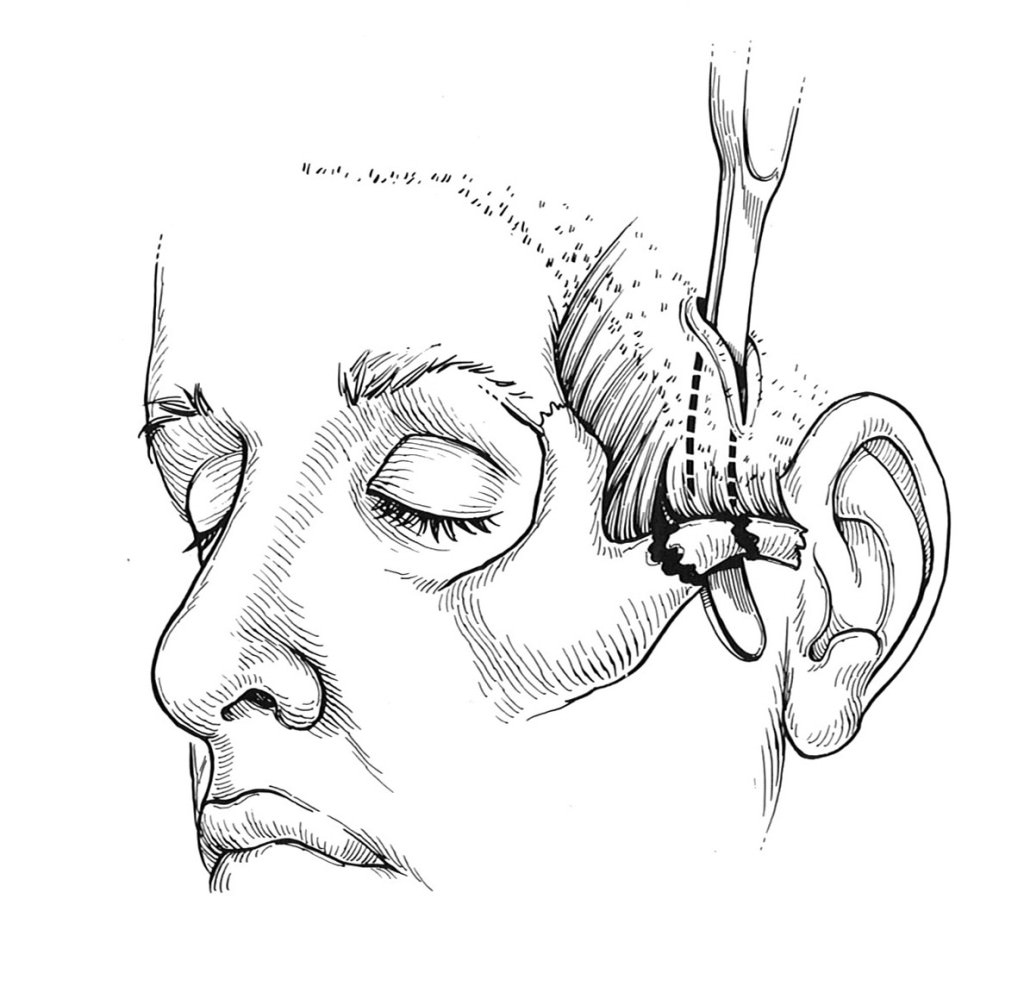
Fracture of the left cheekbone (zygoma). (Illus. from Surgery of Facial Bone Fractures by John E. Sherman MD)
Fractures of the zygoma occur from blunt force trauma either from a fall, motor vehicle accident, or assault. The zygoma (cheekbone) fracture occurs at the maxilla, the zygomatic arch and superior orbital rim articulating in three places.
The illustration above shows a typical cheekbone fracture (fracture of the zygoma) causing downward displacement of the bone. This is often called a tripod fracture because of the three locations of the fractures. The bone is usually displaced downward, which may impinge on the movement of the upper jaw (maxilla).
Facial Anatomy of the Cheekbones
The cheekbones are bones that involve the area around the orbit of the eye (beneath and around the eye socket), the zygoma, zygomatic arch, and the maxilla. The zygomatic arch is the bone area that connects the under-bone of the eye to the area below the temple just before (anterior to) the ear. A tripod fracture is a facial fracture that involves the zygoma, which is displaced. It may involve the arch and the orbit.
Symptoms of Fractures of the Zygoma
Cheekbone fractures often are painful if they are displaced. Often the individual that has the cheekbone fracture will find that chewing, talking, yawning or anything having to do with the movement of the face in that area will be painful. The additional fracture pain is due to the compression of the zygoma (cheekbone area) on the muscles that are below.
Case 1

Figure A” shows a 50-year-old patient who fell sustaining a bilateral LeFort III facial fracture. He incurred fractures of right and left maxillae, zygoma (cheekbone) and orbital floors.
Case 2
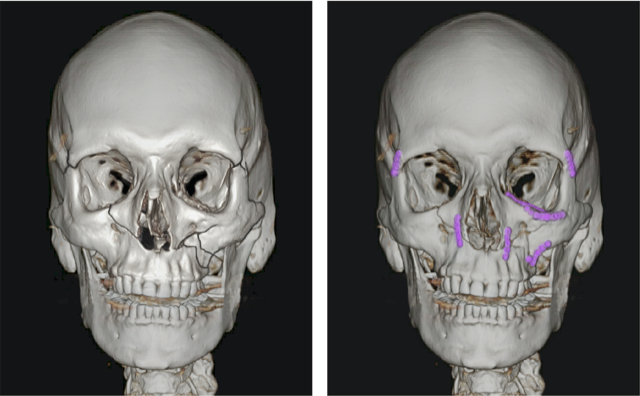
Figure “B” shows repair of the multiple facial fractures. An orbital floor implant was required on the patient’s left side, and multiple plates over the cheekbones and maxilla (upper jaw) and orbit.
The area of the cheek extending to the teeth of the maxilla (upper jaw) may also be numb. This is due to the injury to the infraorbital nerve which is often involved at the fracture site. Sensation usually returns up to nine months later.
Diagnosis of these injures is made after a CT scan. If you have an orbital injury, an ophthalmologist should also examine the eye to make sure that there is no damage to the globe.
Case 3
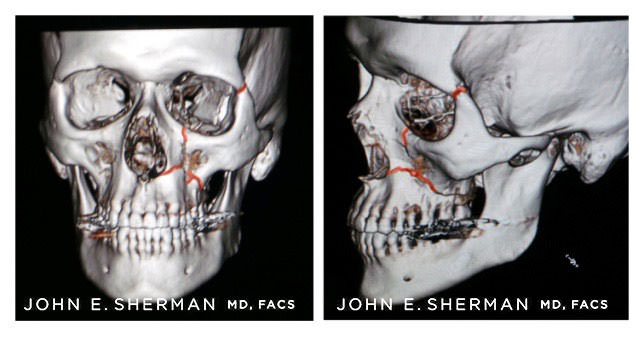
Preoperative scan of 29 year old male victim of assault, who sustained fracture of the zygoma. Fracture lines are highlighted in red.
Postoperative view showing reduction of the fracture with titanium plates, restoring normal anatomy (highlighted in blue).
Arch Fracture
A fracture may often only involve the arch of the zygoma. The most significant symptom is trismus, pain caused by opening the mouth. The treatment for this is different than full fractures of the zygoma. A small incision is made behind the hairline, and an instrument is inserted to simply elevate the displaced fragment.
Complex Facial Fractures
Actual Patient Review
I am fortunate to have been lined up with Dr. Sherman. My 20 yr. old son Jack was in a horrific accident March 10th 2023 up in Canada while snowmobiling.Severe Skull & Facial fractures along with traumatic brain injury. After 9 days in ICU up in Canada we air lifted him back to NY Weill Cornell Hospital. We were introduced to Dr. Sherman through the Neuro surgeon. Dr. Sherman was very thorough and confident.Dr. Sherman reconstructed his whole left side of his face. Jack has approximatley 10 brackets holding all his facial bones back in place. Surgery was about 10 1/2 hrs long. Jack Is Back, looks almost perfect. Dr. Sherman was truly amazing. While going through the worst time as a parent, Dr. Sherman made us feel very at ease & comfortable.He explained the surgery in detail. He is 100% invested into his trade and is truly compassionate. He obviously loves what he does and i would definatley recommend him. Also he is very attentive and easy to contact at any given time. That alone is unheard of. Thank You Dr. John Sherman!!!
Case 1
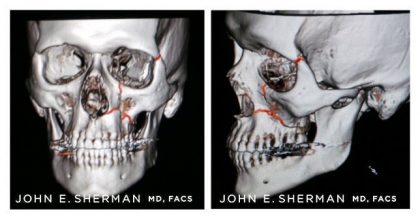
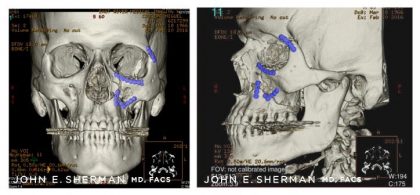
25 year old male who fell from second story window, sustaining Le Fort III multiple facial fractures of the maxilla, mandible, midface and both orbits. Dr. John Sherman led his multispecialty team in reestablishing normal facial anatomy.
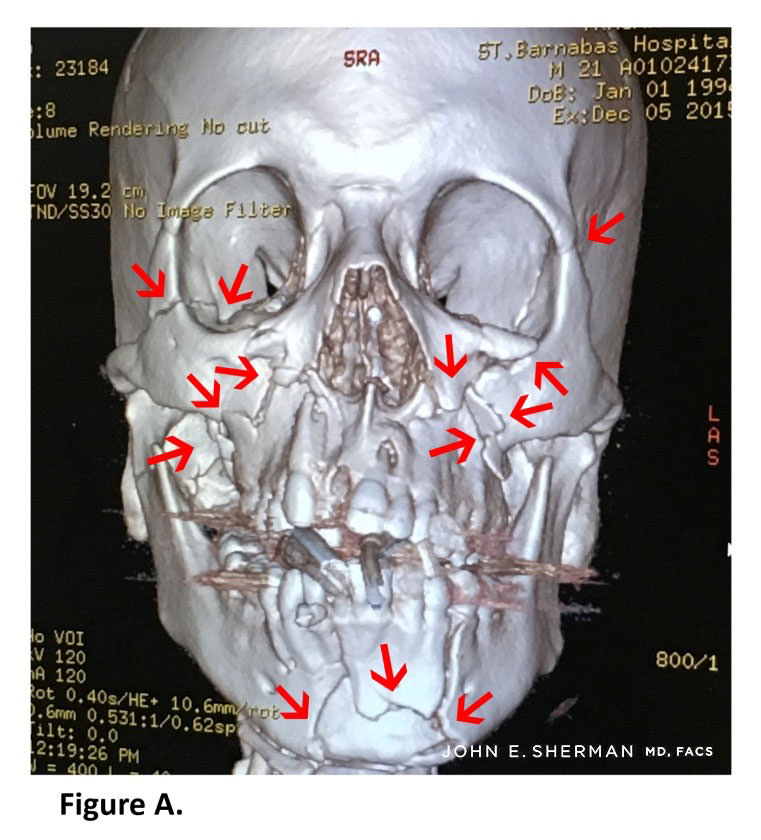
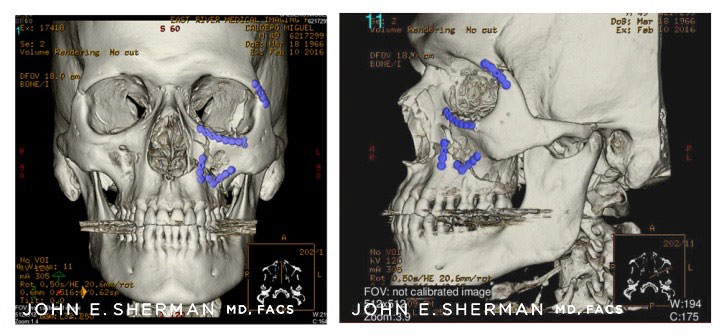
Figure A. Red arrows show size of fractures throughout maxilla, mandible, orbit and zygoma.
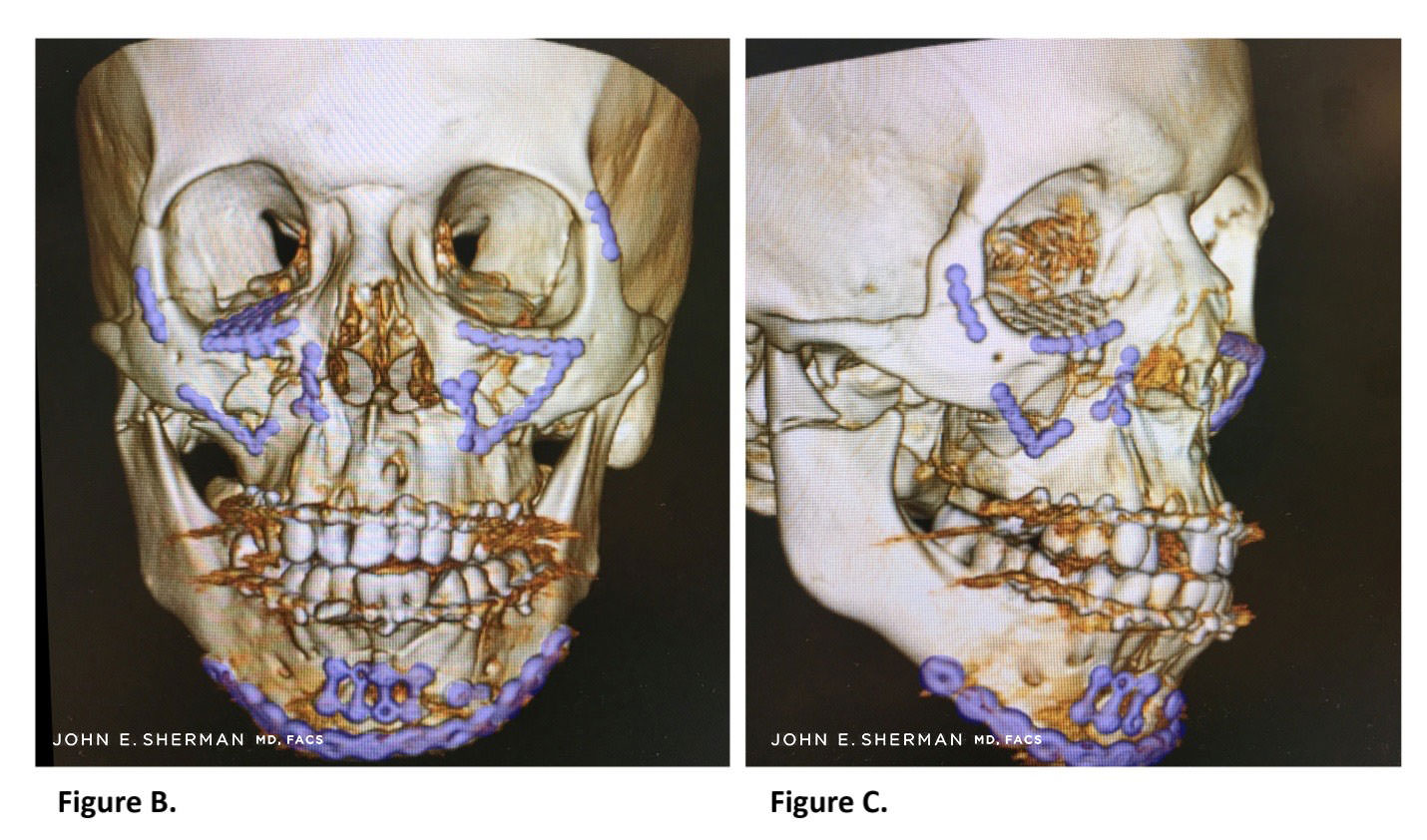
Figure B, C. Reduction and occlusion were restored after the fixation with multiple screws and plates. Images show position of plates (highlighted in blue) after complex surgery to repair Le Fort III fracture, restoring normal facial anatomy.
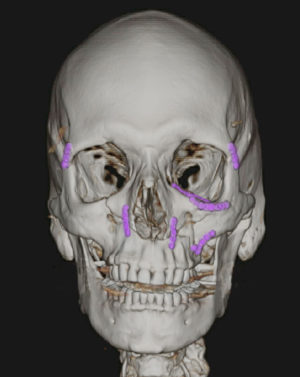
Case 2

Above images depict severe facial bone trauma and subsequent repair in a 39-year-old patient who suffered a four-story fall.
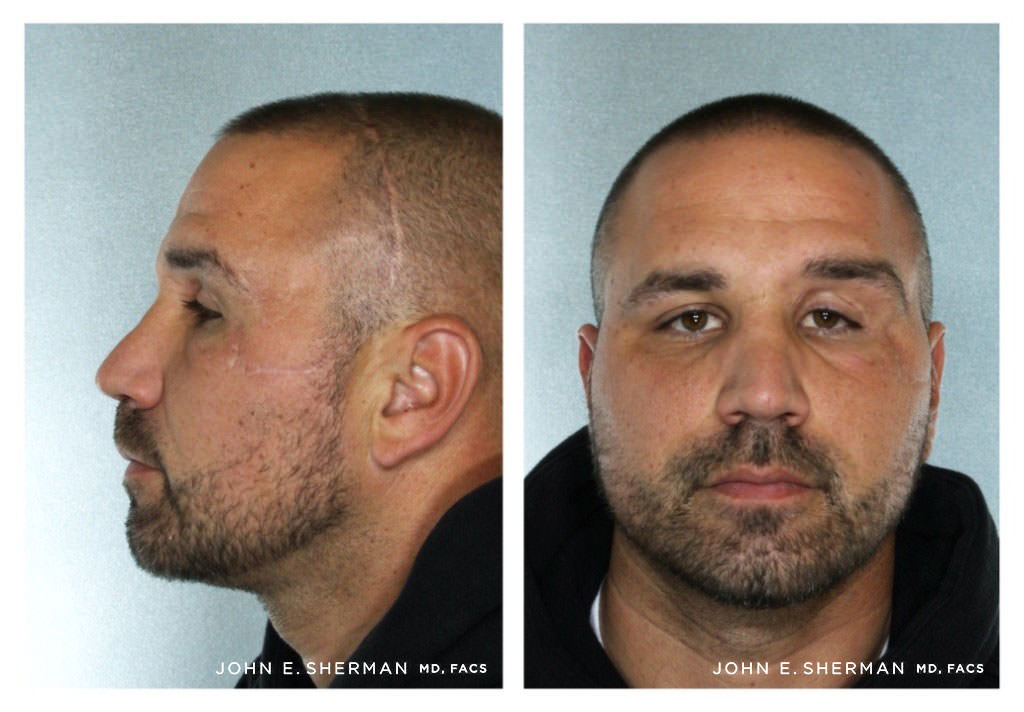
Post-operative images of above patient after successful bone reconstruction following severe trauma.
Treatment of Complex Facial Fractures
The patient must be evaluated to ensure that no other injuries are present. Orthopedic surgeons, critical care physicians, and neurosurgeons are often involved in the treatment of the more complex injuries.
Surgery is usually performed after hospital admission and the patient is stabilized. Remarkably, after the fractures are stabilized, pain is modest and the patient feels better because there is no more movement of the involved bones.
Access incisions may be made in the mouth, eyelid (transconjunctival) and the brow. More complex fractures may involve incisions behind the hairline.
If you have suffered from a cheek fracture, facial trauma, or have previous facial injury, contact our office to schedule your consultation with Dr. Sherman, a world renowned facial trauma specialist, today. If you are hospitalized, transfer to the New York Presbyterian hospital can be arranged.